
Authored by Maria Sampani
October is the Breast Cancer Awareness Month, stressing out the importance of early detection and proper treatment.
What is breast cancer?
Breast cancer is a disease in which cancer (malignant) cells form in the breast tissues. Most types of cancer cells eventually form a lump or mass called a tumor, and are named after the part of the body where the tumor originates, as well as the type of cell. There are two types of (original) breast cancer: the ductal carcinoma, which is more common, and the lobular carcinoma. In the ductal carcinoma, the cancer begins in the lining of milk ducts, while in the lobular it begins in the lobules (milk glands) of the breast. Invasive breast cancer occurs when the cancer has spread from the initial points (milk ducts or lobules) to surrounding normal tissue. Breast cancer affects both men and women, in a ratio of 1:150.
Breast cancer facts
Breast cancer is the most common cancer in women worldwide and the second most common cancer overall. There are 2 million new cases in 2018 and approximately 460,000 deaths from breast cancer each year. It affects 1 in every 8 women, and 1 in every 1,000 men. In the US, every 2 minutes a woman is diagnosed with breast cancer and every 13 minutes a woman dies of breast cancer. Early detection is the cornerstone of breast cancer control, increasing tremendously the chances of survival.
Anatomy of the breasts
- The breast consists of
- Mammary (Milk) glands (lobules) that produce and supply milk.
- Milk ducts that transfer milk from the lobules to the nipple.
- Nipple.
- Areola (pink/brown pigment surrounding the nipple).
- Adipose tissue.
- Connective tissue.
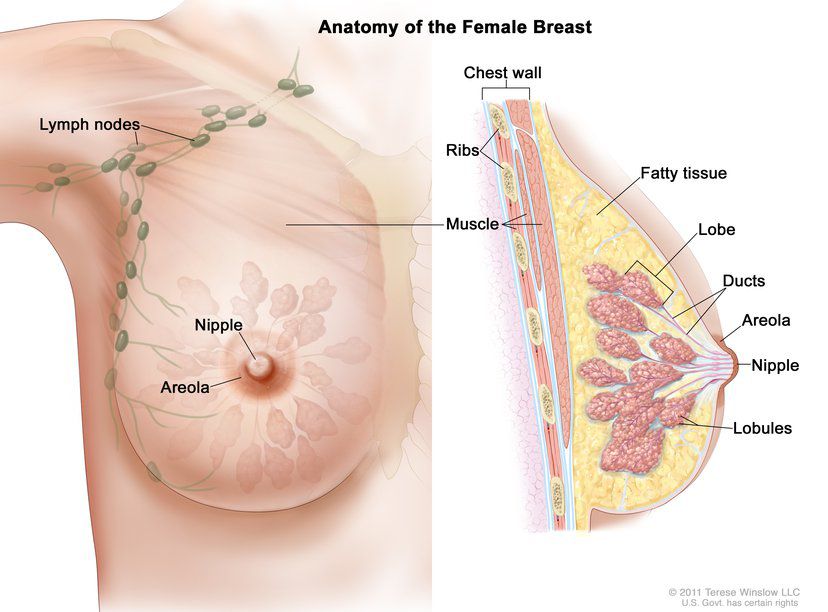
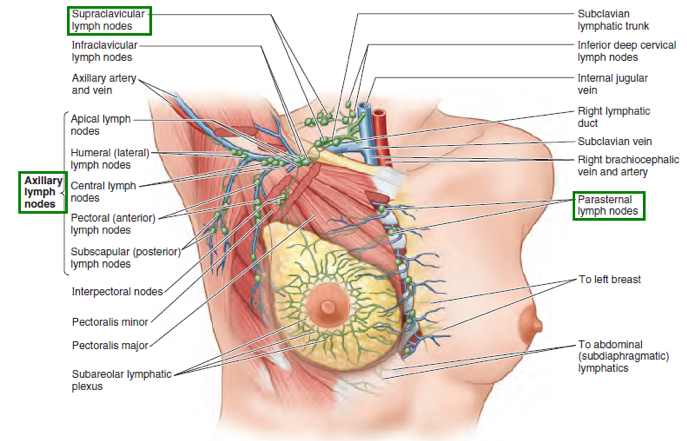
The female adult breast is composed of 15-20 lobes, which are made up of many smaller lobules and surround the nipple in a radial manner. Lymph nodes are located in the armpits (axillary lymph nodes), above the clavicle (subclavicular nodes), and in the chest (parasternal nodes). Lymph runs from the nipple, areola and lobules into a special network, which then drains to the axillary, subclavicular and parasternal lymph nodes.
The growth and development of the breast depends on hormones produced by the ovaries, namely estrogen and progesterone, and on growth hormone. Estrogen elongates the milk ducts and causes them to create branches, while progesterone increases the number and size of the lobules in order to prepare the breast for nourishing the baby.
What are the signs and symptoms of breast cancer?
When the tumor is small it is most easily treated, but at this stage typically there are no symptoms, which is why screening, that allows early detection, is fundamental.
The most common sign is a painless mass, especially if it is hard and irregular, and most importantly if it is tethered or fixed to the underlying chest wall. On the other hand, masses with cystic appearance or painful masses are less likely to be cancerous. Sometimes, the cancer can spread to the axillary lymph nodes and cause a lump or swelling, even before the original breast tumor is large enough to be felt.
Other less common signs and symptoms are: breast pain, swelling of all or part of the breast, skin irritation, redness, scaliness and nipple abnormalities: retraction (turning inward), erosion, spontaneous discharge (especially if bloody). Any persistent change in the breast should be evaluated by a physician as soon as possible.
Diagnosis
The breast cancer can only be diagnosed by biopsy of the nodule. With specific algorithms that calculate the likelihood of diagnosis, unnecessary biopsies are avoided.
Usually, breast cancer is detected during an examination (mammography), before symptoms have developed (screening mammography), or after a woman palpates a mass (diagnostic mammography). Most of the times, the tumors are benign (non-cancerous). However, false positive and false negative results are possible.
Stages
The correct staging of breast cancer patients permits an accurate prognosis and a therapeutic decision-making based on the TNM classification (primary tumor, regional nodes, metastasis). When the T, N and M are determined, a stage of 0, I, II, III or IV is assigned, with stage 0 being in situ (cancer cells are present as a tumor, but have not metastasized, or invaded, beyond the basement membrane of where the tumor was originated), stage I being early-stage invasive cancer, and stage IV being metastasized cancer.
Specifically:
- Stage 0: noninvasive breast cancer in situ, can be either ductal carcinoma in situ (DCIS) or lobular carcinoma in situ (LCIS), also known as lobular neoplasia.
- Ductal Carcinoma In Situ: the majority of in situ cases, in which malignant cells replace the normal epithelial cells lining the milk ducts. DCIS may or may not progress to invasive cancer, but there is an increased risk compared to LCIS.
- Lobular Carcinoma In Situ: malignant cells grow within the lobules of the breasts. It can be considered a premalignant condition with associated elevated risk for subsequent breast cancer, rather than a form of malignancy itself.
- Stage I: early-stage invasive cancer; malignant cells invade normal surrounding breast tissue.
- Stage II: invasive cancer, might have spread to (axillary) lymph nodes.
- Stage III: late-stage invasive cancer, has spread to (axillary) lymph nodes.
- Stage IV: metastatic cancer; invasive breast cancer that has spread beyond the breast and nearby lymph nodes to other organs of the body, distant lymph nodes, skin, bones, liver or brain.
The majority of breast cancer cases (80%) are invasive. Though, there is diversity in terms of risk factors, presentation, response to treatment, and outcomes, because there are up to 21 distinct histological subtypes and at least 4 molecular subtypes. Molecular subtypes are categorized identifying the presence or absence of hormone (estrogen/progesterone) receptors (HR+/HR-), excess level of human epidermal growth factor receptor 2(HER2) and/or extra copies of the HER2 gene (HER2+/HER2-).
The 4 basic molecular subtypes are:
- Luminal A (HR+/HER2-) (71%): Slow-growing, less aggressive, low grade and associated with the most favorable prognosis.
- Triple negative (HR-/HER2-) (12%): More common in black women, in premenopausal women and those with the BRCA1 gene mutation. It has the poorest prognosis and there are no targeted therapies.
- Luminal B (HR+/HER2+) (12%): Tend to be higher grade and are associate with poorer survival than luminal A cancers.
- HER2 amplified (HR-/HER2+) (5%): Most aggressive type, though there are targeted therapies.
Risk factors
Breast cancer is a multifactorial disease, associated with age, sex, hormones, environment, race, habits, obesity, radiation and genetic factors. Specifically, 75% of all breast cancers is found in women over 50 years, and as was mentioned, the female to male ratio is approximately 150:1.
Women without functioning ovaries, who experience an early menopause, and who have never received combination estrogen/progesterone replacement therapy have a lower risk of developing cancer. On the other hand, women with early menarche, late first full-term pregnancy and late menopause, have a higher risk. Environmental factors play an important role and sometimes overshadow the racial ones; immigrants can adopt the prevalence of their new home-country. Dietary fat uptake, is associated with higher risk, but the mechanism might be indirect. Obesity, alcohol consumption, depression, exogenous use of female hormones, oral contraceptives (combination of estrogen and progesterone), hormone replacement therapy, and radiation are all carcinogenetic.
Concerning the genetic factors, they can be either inherited or acquired. Inherited germline susceptibility and environmentally driven somatic changes, eventually lead to potential malignancy. Less than 10% of human breast cancers can be linked directly to a single germline single nucleotide polymorphism (SNP). The most clinically related genes are the BRCA1 and BRCA2 genes. Women with the BRCA1 mutated allele have a 60-80% lifetime chance of developing breast cancer and 33% chance of developing ovarian cancer. Almost non-exceptionally, cancers arising within a BRCA1-mutated patient, are “triple negative” breast cancers. BRCA2-mutated gene is also a risk factor for developing breast cancer in women. The causes of acquired mutations in genes are not yet known. An acquired p53 mutation is present in 40% of the cases and an acquired PTEN mutation in 10% of the cases. Overexpression of the ER (estrogen receptor) occurs in 80% of the breast cancers, overexpression of the oncogene erbB2 occurs in 25% of the cases.
Prevention
The prevention of breast cancer can be achieved through lifestyle changes, pharmacological interventions (chemoprevention) and prophylactic surgery. Although a healthy lifestyle is always recommended, it hasn’t been proven to decrease the breast cancer risk. Drugs (tamoxifen, raloxifene) are administered only to high-risk post-menopausal women and lower one-third to one-half the risk, though not in all types of breast cancer. They block estrogen in some tissues and act like estrogen in others. Preventive mastectomy (unilateral/bilateral) is performed on high-risk patients and reduces the risk of breast cancer incidence and mortality by more than 95%. The remaining percentage occurs, because it is not possible to remove all the breast tissue; breasts are not encapsulated organs, therefore some normal tissue is always left behind.
Screening
It’s been a controversial issue how often should a woman be examined with a screening method, but the recommended technique for standard risk women is mammography.
Mammography
It’s a breast imaging technique that uses low-dose x-rays to visualize the internal structure of the breast. Diagnostic mammography is performed after a palpable abnormality has been detected, while the screening mammography is performed in a woman without symptoms or prediscovered abnormalities. There are 3 types of mammography: screen-film, digital and digital breast tomosynthesis. The American Cancer Society (ACS) recommends for women at average risk that those 40-44 years have the option to begin annual mammography, those 45-54 should undergo annual mammography and those 55 years and older can transition to biennial mammography or continue with annual mammographies. If a woman has less than 10 years life expectancy or is not in a good health, the disadvantages of mammography outweigh the benefits, thus screening is avoided. Mammography enables early detection of cancer, reducing the risk of dying from breast cancer by 20% (some studies suggest more than 40%). Though, mammography has flaws: possible false positive and false negative results can be found, overdiagnosis and radiation exposure.
Magnetic resonance imagining (MRI)
It’s recommended for women at increase risk. The women at high lifetime risk (at least 20-25%) should begin at 30 years to be screened annually by both mammography and MRI. Women at moderately high lifetime risk (15-20%) need to consult their doctor for the potential benefits and harms of adding the MRI screening to their annual mammography. Women with less than 15% lifetime risk should not use MRI because it’s more harmful than beneficial.
Breast Ultrasound
Is used to evaluate abnormal findings from a physical exam or a mammogram. It’s not recommended to replace the mammogram because it increases the likelihood of false-positive results.
Clinical Breast Examination (CBE)
It isn’t recommended any more for asymptomatic women with average risk, either alone or in addition to mammography; it doesn’t detect an important proportion of breast cancer tumors and, as the ultrasound, it increases the probability of false-positive results.
Self-examination
All women should be familiar with the appearance and feel of their breasts and be able to detect any change. A palpable mass or a change in the appearance should be reported to the physician. Most masses are benign, and for menstruating women, they appear and disappear within the menstrual cycle.
Treatment
The treatment plan is decided jointly by the patient and the physician based on prognostic and predictive factors, taking into consideration the stage and the type of the cancer, the patient’s age and menopausal status, and the risks and benefits of each therapeutic scheme. One important factor to consider is whether the patient has distant (outside the breast, chest wall, and regional lymph nodes) metastases, detected by scintigraphy or radiography and biopsy, or if he/she doesn’t, in which case the treatment is either therapeutic or life prolongating.
The therapy can be either primary or systemic. Primary therapies consist of surgical and radiation treatments directed toward the breast and locoregional lymph nodes, targeting to excise and eliminate the cancer and sterilize unaffected breast tissue. Adjuvant systemic treatments consist of antiestrogen (or endocrine), anti-HER2, and/or chemotherapies, which are given to treat micrometastases that have invaded distant sites but are not detectable yet.
The surgical treatment can be either breast-conserving surgery or mastectomy (unilateral/bilateral). In breast-conserving surgery, the cancerous tissue and the tumor margin are removed, and in most cases radiation therapy follows. However, not all the patients are eligible. Mastectomy is the removal of the entire breast. Another, less common practice is the modified radical mastectomy, which includes a full dissection of axillary lymph nodes on top of the entire breast removal. Many women who are eligible for breast conserving surgery opt for mastectomy, and some that are diagnosed with breast cancer in only one breast choose to have the unaffected breast removed as well (contralateral prophylactic mastectomy or bilateral mastectomy). In both breast-conserving surgery and mastectomy, at least one axillary lymph node is removed and examine to determine whether the cancer has spread beyond the breast. In many cases, breast reconstruction is following mastectomy, either in the same surgery, or at any time.
Radiation therapy is the use of high-energy beams or particles to kill cancer cells and most of the times it’s following surgery, in order to destroy the remaining cancer cells.
Systemic therapy is administered through bloodstream, to treat all parts of the body. Chemotherapy attacks fast-growing cells, such as cancer cells, anti-estrogen therapy either blocks the body’s natural hormones or lowers their levels, and HER2 therapy attacks specific molecules active in cancer cells.
Survival
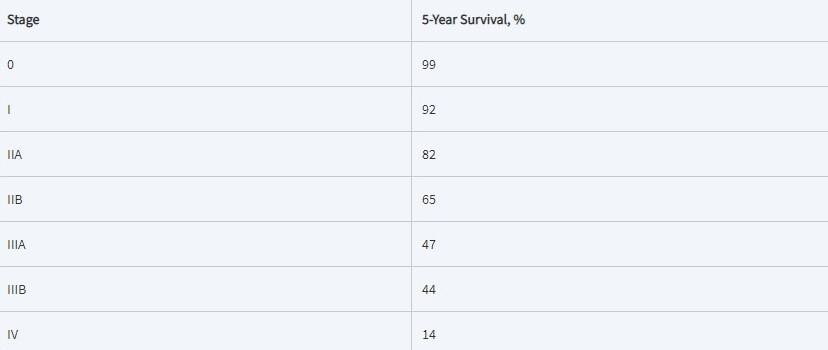
Relative survival rate is the estimated percentage of patients who will survive for a given period of time after diagnosis, compared to life expectancy for people of the same age and race, that aren’t diagnosed with cancer. Relative survival rates for women diagnosed with breast cancer are: 91% 5 years after diagnosis, 86% after 10 years and 80% after 15 years. Attention should be given to the data, because every individual is unique and the data are long-term, which means that they were calculated when the diagnosis and treatment of breast cancer were poorer. Survival rate depends on the stage of the cancer at diagnosis and the ethnicity of the patient. The racial disparity in survival reflects later stage at diagnosis and poorer stage-survival in black women and higher rates of more aggressive, triple negative breast cancer. The racial gap, though, seems to be narrowing.
5-year survival rate for breast cancer by stage:
There are still many “missing pieces” when it comes to breast cancer, but the future is full of potentials.


